Estimated Prevalence and Cost of Diabetes
|
Prevalence (1) |
2023 |
2033 |
|---|---|---|
|
Diabetes (type 1 + type 2 diagnosed + type 2 undiagnosed) |
2,409,000 / 15% |
3,009,000 / 17% |
|
Diabetes (type 1 and type 2 diagnosed) |
1,686,000 / 11% |
2,106,000 / 12% |
|
Diabetes (type 1) |
5-10% of diabetes prevalence |
|
|
Diabetes (type 1 + type 2 diagnosed + type 2 undiagnosed) and prediabetes (includes undiagnosed) |
4,808,000 / 30% |
5,722,000 / 33% |
|
Increase in diabetes (type 1 and type 2 diagnosed), 2023-2033 |
25% |
|
|
Direct cost to the health care system |
$1.7 billion |
$2.1 billion |
|
Out-of-pocket cost per year (2) |
||
|
Type 1 diabetes costs, % of family income |
$694-$5,245 / 2%-17% |
|
|
Type 2 diabetes costs, % of family income |
$287-$4,985 / 1%-17% |
|
Impact of Diabetes
- Among Ontarians (1):
- 30% live with diabetes or prediabetes, and
- 11% live with diagnosed diabetes, a figure that climbs to 15% when cases of undiagnosed type 2 diabetes are included.
- Diabetes contributes to (5):
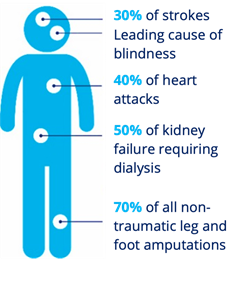
- Diabetes complications are associated with premature death (3). Diabetes can reduce lifespan by five to 15 years (3). It is estimated that the all-cause mortality rate among Canadians living with diabetes is twice as high as the all-cause mortality rate for those without diabetes (4).
- People with diabetes are over three times more likely to be hospitalized with cardiovascular disease, 12 times more likely to be hospitalized with end-stage renal disease, and almost 20 times more likely to be hospitalized for a non-traumatic lower limb amputation compared to the general population (3).
- 33-50% of people living with diabetes experience diabetes distress (an overwhelming feeling about their condition that can lead to unhealthy habits like not checking their blood sugar or skipping medical appointments, etc.) (6).
- Individuals with depression have a 40% – 60% increased risk of developing type 2 diabetes (6).
- Diabetic retinopathy, a retinal vascular disorder that occurs as a complication of diabetes, is a leading cause of new cases of blindness in Canada, and often affects working-aged adults (7).
- Vision loss is associated with significant morbidity, including increased falls, hip fractures, and an increased risk of death (8).
- Foot ulceration affects an estimated 15-25% of people with diabetes in their lifetime (9).
- Compared to the general population, adults living with diabetes in Canada are over 20 times more likely to undergo non-traumatic lower limb amputations - 85% of which are preceded by foot ulcers (10).
- Hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) may affect mood and behaviour and can lead to emergency situations if left untreated (11).
- For people living with diabetes, adherence to treatment is affected by costs which are not covered by their public drugs and devices coverage (2).
- Those with type 1 diabetes can pay up to 17% of their gross annual income on medications and devices that range from $694 to $5,245.
- Those living with type 2 diabetes can pay up to 17% of their gross annual income on medications and devices that range from $287 to $4,985.
Risk Factors for Diabetes
- The risk factors for type 1 diabetes are not well understood, but interaction between genetic and environmental factors are likely involved (11). Type 2 diabetes is caused by a combination of individual, social, environmental, and genetic factors (11).
- Certain populations are at higher risk of developing type 2 diabetes, such as those of African, Arab, Asian, Hispanic, Indigenous, or South Asian descent, those who are older, have a lower level of income or education, are physically inactive, or are living with overweight or obesity (11).
- The age-standardized prevalence rates for diabetes are 16% among people of South Asian descent, 13.3% among Black adults, 12.5% among people of Arab/West Asian descent, 8.8% among people of East/Southeast Asian descent, and 5.7% among people of Latin American descent (12).
- The prevalence of diabetes among First Nations adults living off reserve, Metis adults, and Inuit adults is 1.72 times,1.22 times, and 1.18 times higher respectively than the prevalence among non-Indigenous adult (12). In addition to the risk factors that impact all people in Canada, the ongoing burden of colonization continues to influence Indigenous peoples’ health.
- The prevalence of diabetes among adults in the lowest income groups is 2.1 times that of adults in the highest income group (12).
- Adults who have not completed high school have a diabetes prevalence 1.9 times that of adults with a university education (12).
- Social determinants of health can influence the rate of individual-level modifiable risk factors and thus the risk of diabetes. The main determinants of health include income, employment, education, childhood experiences, physical environments, social supports, access to health services, and racism (13).
Policy, Programs, and Services Related to Diabetes
- In April 2023, a motion was unanimously passed in the Ontario Legislature asking the Minister of Health and Ontario Health to develop a provincial framework on chronic diseases with an initial focus on diabetes.
- Effective March 2022, the Assistive Devices Program (ADP) provides coverage for real-time continuous glucose monitoring systems (rtCGM) for Ontario residents with type 1 diabetes who have had a severe hypoglycemic event or cannot recognize or communicate the symptoms of hypoglycemia.
- In November 2021, the government expanded public funding of intermittently-scanned continuous glucose monitoring systems (isCGM) to include Freestyle Libre 2 for all Ontario Drug Benefit clients who use insulin and have a valid prescription from their physician or nurse practitioner.
- In September 2019, the government announced public funding for intermittently-scanned continuous glucose monitoring systems (isCGM) for all Ontario Drug Benefit clients who use insulin and have a valid prescription from their physician or nurse practitioner.
- In November 2017, the government announced funding of $8 million over three years and continues to fund offloading devices to help improve patient outcomes and reduce the risk of amputation for Ontarians with diabetic foot ulcers.
- OHIP+ provides more than 4,400 drug products at no cost for Ontarians 24 years or younger who are not covered by a private plan.
- Seniors 65 years or older, and individuals/families with high-prescription drug costs relative to their income, may receive coverage for prescription drugs through Ontario Drug Benefit and Trillium Drug Program; deductibles and co-pays apply.
- The Monitoring for Health Program provides assistance with the cost of blood glucose testing supplies for Ontarians who use insulin or have gestational diabetes and have no other coverage for their supplies. The maximum reimbursement for strips and lancets is $920 per year.
- The Insulin Syringes for Seniors Program provides $170 annual grant to help with the cost of pen needles/syringes for seniors 65 years or older who use insulin.
Challenges
Ontario faces unique challenges in preventing type 2 diabetes and meeting the needs of those living with diabetes:
- Non-modifiable risk factors of type 2 diabetes include age, gender, and ethnicity (11).
- 16.7% of Ontarians are over 65 years old (14). The risk of developing type 2 diabetes increases with age (11). Older adults living with diabetes are more likely to be frail and progressive frailty has been associated with reduced function and increased mortality (15).
- Adult men are more at risk of type 2 diabetes compared to adult women (11).
- Approximately 32.2% of Ontarians self-identify as being of African, Arab, Asian, Hispanic, or South Asian descent (14). These groups are at increased risk of developing type 2 diabetes (11).
- There are 374,395 Indigenous people in Ontario, who face significantly higher rates of diabetes and adverse health consequences than the overall population (16).
- Ontario has high rates of individual-level modifiable risk factors (17):
- 43.4% of adults and 74.1% of youth aged 12 to 17 are physically inactive;
- 35.9% of adults are living with overweight and 26.2% of adults are living with obesity;
- 73.2% of adults are not eating enough fruits and vegetables; and
- 17.1% of adults are current tobacco smokers.
- The strict criteria of the Ontario Assistive Devices Program (ADP) results in many individuals who may benefit from use of a rtCGM.
- Factors related to the social determinants of health and that can influence the rate of individual-level modifiable risk factors among Ontarians include income, education, food security, the built environment, social support, and access to health care (3).
- Ontario has one of the highest prevalence of low income among all provinces, based on low-income cut-offs after tax (18). People with diabetes earning a low income may face financial constraints that can make their disease more difficult to manage.
- People living with diabetes in Ontario continue to face high-out-of-pocket costs, to manage their diabetes effectively. This is especially the case for those who do not have coverage for their diabetes medications, supplies, or devices through Ontario’s publicly funded programs or private plan. However, even with coverage, many Ontarians face significant out-of-pocket costs due to high public drug program deductibles (e.g., Trillium Drug Program), lack of public funding for diabetes devices (e.g., Continuous Glucose Monitoring systems) and essential diabetes supplies (e.g., insulin pen needles), and/or annual limits on coverage through private plans.
Diabetes Canada’s Recommendations to the Government of Ontario
- Fund a provincial diabetes framework
- Allocate funding to develop and implement a comprehensive diabetes framework with measurable goals for improving diabetes prevention, treatment and health outcomes for the province.
- Expand access: Put patients at the centre of policy decisions
- Eliminate barriers, including age discrimination, to access evidence-based, personalized diabetes treatments, including diabetes medications, devices, and supplies.
- Provide equitable access to continuous glucose monitoring systems (isCGM & rtCGM) according to Diabetes Canada’s reimbursement recommendations.
- Protect students with diabetes
- Implement a mandatory standard of care for students with diabetes that aligns with Diabetes Canada’s Guidelines for the Care of Students Living with Diabetes at School.
- Prevent amputations
- Implement health policies that support the prevention and management of diabetes foot complications and reduce the risk of lower limb amputations.
References
- Canadian Diabetes Cost Model. Ottawa: Diabetes Canada; 2016.
- Diabetes and Diabetes-Related Out-of-Pocket Costs: 2022 Update. Diabetes Canada; 2022.
- Diabetes in Canada: Facts and figures from a public health perspective [Internet]. Ottawa: Public Health Agency of Canada; 2011 p. 126. Available from: https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres-2011/pdf/facts-figures-faits-chiffres-eng.pdf
- Public Health Agency of Canada. Twenty years of diabetes surveillance using the Canadian chronic disease surveillance system. [Internet]. 2019. Available from: http://publications.gc.ca/collections/collection_2019/aspc-phac/HP35-122-2019-eng.pdf
- Hux J, Booth J, Slaughter P, Laupacis A. Diabetes in Ontario: An ICES Practice Atlas [Internet]. Institute for Clinical Evaluative Sciences; 2003. Available from: https://www.ices.on.ca/Publications/Atlases-and-Reports/2003/Diabetes-in-Ontario
- Diabetes Canada Clinical Practice Guidelines Expert Committee, Robinson DJ, Coons M, Haensel H, Vallis M, Yale JF. Diabetes and Mental Health. Can J Diabetes. 2018 Apr;42 Suppl 1:S130–41.
- Flaxel, Christina J.; Adelman, Ron A.; Bailey, Steven T.; Fawzi, Amani; Lim, Jennifer I.; Vemulakonda, G. Atma; Ying, Gui-shuang. Ophthalmology (Rochester, Minn.), 2020, Vol.127 (1), p.P66-P145
- Vu, H. T., Keeffe, J. E., McCarty, C. A., & Taylor, H. R. (2005). Impact of unilateral and bilateral vision loss on quality of life. The British journal of ophthalmology, 89(3), 360–363. https://doi.org/10.1136/bjo.2004.047498
- Yazdanpanah, L., Shahbazian, H., Nazari, I., Arti, H. R., Ahmadi, F., Mohammadianinejad, S. E., Cheraghian, B., & Hesam, S. (2018). Incidence and Risk Factors of Diabetic Foot Ulcer: A Population-Based Diabetic Foot Cohort (ADFC Study)-Two-Year Follow-Up Study. International journal of endocrinology, 2018, 7631659. https://doi.org/10.1155/2018/7631659
- Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. N Engl J Med. 2017 Jun 15;376(24):2367–75
- Diabetes Canada Clinical Practice Guidelines Expert Committee. Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Can J Diabetes. 2018;42(Suppl 1):S1:S325.
- Public Health Agency of Canada. Pan-Canadian Health Inequalities Data Tool, 2022 Edition [Internet]. Available from: https://health-infobase.canada.ca/health-inequalities/data-tool/
- Prinjha S, Wicklow B, Nakhla M, Banerjee AT. Toward the Goal of Understanding and Tackling the Social Determinants of Diabetes. Can J Diabetes. 2022 Aug 1;46(6):549–50.
- Government of Canada SC. Census Profile, 2016 Census - Ontario [Province] and Canada [Country] [Internet].
- Meneilly GS, Knip A, Miller DB, Sherifali D, Tessier D, Zahedi A. Diabetes in Older People. Can J Diabetes. 2018 Apr;42:S283–95.
- Aboriginal peoples in Canada: Key results from the 2016 Census [Internet]. Ottawa: Statistics Canada; 2017 Oct p. 11. Available from: https://www150.statcan.gc.ca/n1/en/daily-quotidien/171025/dq171025a-eng.pdf?st=krvs_yCt
- Canadian Risk Factor Atlas (CRFA), 2020 edition. Public Health Agency of Canada. Available at Public Health Infobase: https://health-infobase.canada.ca/crfa/
- Table 11-10-0136-01 Low income statistics by economic family type [Internet]. Ottawa: Statistics Canada; 2019 Dec. Available from: https://doi.org/10.25318/1110013601-eng